Occlusive dressing - everything you need to know
Content
- Purpose and goals of using occlusive dressings
- The mechanism of action of the occlusive dressing
- Areas of application of occlusal dressings
- Occlusive dressing for pneumothorax
- Algorithm for applying occlusive dressings
- Step 1: Preparation
- Step 2: Capture the starting point
- Step 3: Wrapping
- Step 4: Fixing
- Step 5: Anchoring and evaluation
- Tips for choosing an occlusive dressing
An occlusive dressing is a means of sealing wounds used in the treatment of chest infections (e.g., in the case of an open pneumothorax). Usually, when the chest is injured, air penetrates into the abdominal cavity, which leads to an equalisation of pressure and breathing difficulties (lung volume decreases and their functionality is impaired).
The use of an occlusive bandage requires an appropriate application technique. We recommend that you read detailed information on the technique and importance of first aid in our article ‘First Aid for Injuries’.
Purpose and goals of using occlusive dressings
There is a variety of methods for covering the damaged area depending on the extent of the injury and the nature of the wound. As for the use of an occlusive dressing, it is effective in open wounds that are characterised by intense bleeding and damage to internal organs. The use of this dressing protects the injured area from friction, impact and external influences that can negatively affect the recovery process.
The occlusive dressing creates an optimal microclimate, where the necessary humidity and temperature are maintained for normal wound healing. At the same time, the sterile dressing is absorbent, protecting the damaged surface from toxins, bacteria, contamination and excessive secretions.
An occlusive dressing is usually used in traumatology for bullet wounds. Its use prevents air from reaching the damaged organs, thereby alleviating the condition of the victim. It is also used in surgery for the treatment of postoperative wounds and in dermatology for the treatment of diseases where trophic ulcers appear, such as psoriasis or diabetes mellitus.
An airtight occlusive dressing is an important tool in the treatment of eye injuries (chemical and mechanical damage), as well as in everyday injuries such as burns or deep cuts.
In practice, an occlusive dressing is used primarily to restore the tightness of the pleural cavity. However, due to its sealing properties, it is also used in other areas.
Recently, the occlusive dressing has been used in cosmetology as part of the treatment of acne and pimples, where the ointment ‘Contractubex’ is used to help prevent and resolve scars.
Systematic training in the application of various types of bandages is a whole scientific discipline. As for the specific technique of applying an occlusive dressing, it is described in detail in the ‘Dressing Instructions’ - desmurgia. Knowledge of the dressing algorithm is important for medical professionals of all levels, from nurses to doctors.
The mechanism of action of the occlusive dressing
A material is considered ‘occlusive’ when it keeps the wound surface moist while the dressing is secured in place of the damaged tissue. The successive alternation of layers of synthetic gauze prevents the wound from drying out by preventing water vapour from evaporating from the wound surface into the atmosphere. The process of applying an occlusive dressing allows moisture vapours to dissipate from the wound at a lower rate than they escape, creating a humid environment and promoting the healing process.
Areas of application of occlusal dressings
This wound dressing is used to seal certain types of wounds together with the surrounding tissue, protecting them from air, liquids and harmful contaminants such as viruses and bacteria. This is especially important in the case of injuries or first aid. Often, this material is used to directly control the cleanliness of the wound, as well as to reduce blood loss in cases where inpatient treatment is not available.
The use of an occlusive dressing corrects situations with pneumothorax, and also complements haemostatic measures in cuts and lacerations. In some scenarios, it is also used for open rib fractures and upper respiratory tract injuries.
Occlusive dressing for pneumothorax
In cases of open pneumothorax, it is recommended to apply an occlusive dressing within 10-15 minutes after the injury. Otherwise, additional drainage or preliminary wound soaking with tampons may be necessary to remove blood clots.
Basic steps for applying an occlusive dressing on the chest in case of pneumothorax:
- Close all air inlets and outlets. If there are air inlets and outlets, make sure that both are present and properly treated.
- Leave the final diagnosis to the professionals. Regardless of your perception of the diagnosis, an occlusive dressing should be applied.
- If you are using a non-ventilated occlusive dressing, wait until the patient exhales before applying the dressing.
- If you are unsure, you can squeeze the bandage around the patient while still achieving the sealing objectives.
- If you are using a non-ventilated occlusive dressing and the patient's breathing becomes more difficult over time, you can adjust the process.
- Cover the wound with the dressing as you inhale and open it as you exhale. This action is similar to a ventilated dressing.
Algorithm for applying occlusive dressings
- Clean and dry the area around the wound as much as possible before applying the dressing to the chest.
- Apply damp sterile gauze to the wound to stop bleeding.
- Next, wrap the gauze and wound with an occlusive dressing, pressing the edges carefully to create a secure, airtight seal.
- For chest injuries, wait for the patient to exhale or ask them to cough before applying the dressing. This will help to reduce the amount of air that may be trapped in the chest.
It is important to note that applying an occlusive dressing in the field requires training. It is useful to attend specialised courses or workshops and improve your technique on training dummies or with a partner.
Step 1: Preparation
Preparation for the application of occlusal dressings is critical for the effective wound healing process. First of all, it is necessary to ensure proper cleaning of the wound area with antiseptic agents to eliminate dirt, microorganisms and other contaminants. Next, disinfection should be performed to reduce the risk of infection.
Providing a humid environment is another important part of the preparation. It promotes active healing and rapid tissue recovery. The right dressing material that can retain moisture will help create favourable conditions for healing.
In general, proper preparation before applying occlusal dressings provides optimal conditions for the rapid and effective recovery of damaged tissues.
Step 2: Capture the starting point
This stage determines the reliability and stability of the dressing throughout the treatment period. It is important to choose the right place to grip, preferably choosing stable points in the anatomical structure that allow for even pressure distribution.
When gripping the starting point, care should be taken to ensure proper fixation to avoid shifting or tearing during application. This technique helps to distribute the load evenly on the dressing, avoiding excessive compression or tearing.
Capturing the starting point also affects the tightness of the dressing, which is important for moisture control and infection prevention. In addition, this step plays a role in ensuring patient comfort, as a properly secured dressing does not cause excessive discomfort or restriction of movement.
Therefore, careful and attentive capture of the starting point before applying occlusive dressings has a significant impact on the effectiveness of treatment and wound healing.
Step 3: Wrapping
It is important to follow some key principles.
- Firstly, the wrapping should be even and balanced. Equal pressure over the entire surface of the dressing helps to avoid uneven compression, which can lead to deformation or tearing of the dressing.
- Secondly, it is important to avoid excessive compression. Too much pressure can restrict blood circulation and lead to irritation or even tissue damage. The wrapping should be sufficient to ensure the stability of the dressing, but not to interfere with normal blood circulation.
- Thirdly, the correct direction of wrapping should be observed. Usually, wrapping starts with less vulnerable areas and gradually moves to larger ones. This helps to ensure tightness and even pressure over the entire wound surface.
In addition, taking into account the individual characteristics of the patient, it is important to be careful and avoid excessive tension and discomfort during the wrapping.
Step 4: Fixing
Not only the stability of the dressing, but also the effectiveness of treatment and wound healing depend on proper fixation.
It is important to take into account the individual characteristics of the patient and the nature of the wound when choosing a fixation method. Elastic bandages, special fixing adhesive tapes or adhesive films can be used to ensure a firm fixation. It is important that the fixation material does not restrict movement or cause discomfort to the patient.
For wounds located in hard-to-reach areas, it may be important to use additional fixation devices, such as bandages with special fasteners or bandages with large rings for convenience.
Taking these aspects into account, properly selected and properly secured occlusive dressings help to ensure the necessary tightness, moisture control and protection of the wound from external factors. This approach contributes to a quick and successful healing process, as well as a comfortable experience for the patient during treatment.
Step 5: Anchoring and evaluation
After applying the dressing, it is important to ensure that it is properly secured. This ensures tightness, protection from external factors and optimal healing.
Dressing evaluation involves systematic monitoring of its condition. It is important to pay attention to changes in the colour, texture or smell of the wound. Continuous monitoring allows you to detect signs of infection or insufficient dressing tightness in time.
Ongoing assessment also helps to respond to potential problems in a timely manner. In case of deterioration of the dressing, changes in the wound or other unforeseen events, it is necessary to consult a medical specialist. This approach helps ensure quality care and an effective recovery process.
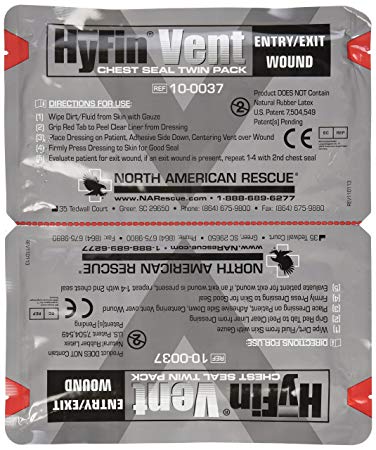
Tips for choosing an occlusive dressing
- First, consider the type of wound. For deep wounds, it is important to choose a dressing that will provide sealing and protection from external infectious agents. For superficial wounds, you can use less airtight options.
- Secondly, the size and position of the wound is important. Some dressings have dimensional options, which allows you to choose the most suitable option for a particular situation.
- Third, pay attention to the material of the bandage. It should be hypoallergenic, allowing you to avoid allergic reactions. It is also important that the bandage fits well and does not cause discomfort.
Do not forget about the individual characteristics of the patient. Some materials may be more suitable for sensitive skin, while others may be more suitable for active people who move a lot.
The choice of an occlusive dressing requires careful consideration and consultation with medical specialists in cases of unclear situations. With the right choice, you can ensure the best conditions for fast and effective wound healing.
