What to do in case of burns and what is the most effective product for their treatment?
Content
- Types of burns
- Symptoms of burns
- What to do with burns at different stages?
- Burn of the 1st degree
- Burn of the 2nd degree
- Burn of the 3rd degree
- Remedies for burns
- What not to use for burn treatment
- Conclusion: preventive tips
Burns are one of the most common household injuries that can happen anywhere: at home, at work, or even while on holiday. Such injuries often occur due to non-compliance with safety rules at work or carelessness at home.
Proper first aid is crucial. How quickly and correctly you react will determine the further condition of the victim and the effectiveness of treatment.
Light burns can heal on their own due to the body's ability to regenerate. However, serious injuries require immediate medical attention to avoid complications, infections and long-term consequences.
In this article, we will tell you what to do in case of burns, what products can help speed up healing, and how to avoid mistakes that can worsen the situation.
Types of burns

Burns can occur for a variety of reasons, and it is important to understand what type of injury you are dealing with in order to help you effectively. Each type of burn has its own characteristics, degree of danger and requires an appropriate approach to treatment.
- Thermal burns. Thermal burns are caused by exposure to high temperatures. They can be caused by flames, hot liquids, steam or hot objects. These injuries are common in situations involving contact with open flames, hot stoves, irons, boiling water or hot metal. In severe cases, deep tissue damage may occur, requiring long-term treatment and special care.
- Chemical burns. This type of burn occurs when the skin or mucous membranes come into contact with aggressive chemicals such as acids, alkalis or toxic compounds. They often occur when working with household chemicals such as pipe cleaners, bleaches, solvents or industrial chemicals. The peculiarity of chemical burns is that the damage can continue even after contact with the substance is stopped, so it is important to rinse the affected area with plenty of water as soon as possible.
- Electrical burns. Electrical burns occur when an electric current passes through the body. Such injuries can be both external and internal, as the current damages tissues along its path. This can happen when you come into contact with bare wires, faulty electrical appliances or lightning. The peculiarity of electric burns is that visible external damage may be minor, while internal organs are severely injured.
- Radiation burns. Radiation burns occur as a result of prolonged exposure to ionising radiation or ultraviolet rays. The most common case is a sunburn, but similar injuries can also occur when exposed to X-rays or other sources of radiation. Radiation burns may not appear immediately, so it is important to monitor the condition of the skin after prolonged exposure to radiation.
Each type of burn has its own characteristics that affect the approach to first aid and subsequent treatment. For example, cooling is a critical step in thermal burns, but it can be ineffective or even harmful in chemical or electrical injuries. Incorrect actions can worsen the victim's condition, exacerbate the injury or cause additional complications.
Symptoms of burns
Symptoms of burns depend on the depth of tissue damage, which determines the severity of the injury. There are four main degrees of burns, each of which has its own characteristic signs. Correctly determining the degree of burn allows you to assess how serious the injury is and determine the need for medical intervention.
First-degree burns are considered the mildest. They affect only the top layer of the skin - the epidermis. The affected area becomes red, there is slight swelling, the skin becomes dry, and there is a burning sensation and pain, especially when touched. Blisters do not form with this lesion. It can be, for example, a sunburn or light contact with a hot surface. Usually, pain and redness persist for 2-5 days, after which the skin begins to peel off, and full recovery occurs without scarring.
Second-degree burns penetrate deeper, affecting not only the epidermis but also the upper layers of the dermis. In this case, the skin becomes bright red, swollen, and accompanied by severe burning pain. A characteristic sign is the formation of blisters filled with clear or cloudy liquid.
After they break, a moist, shiny skin surface remains, which is very sensitive to any irritants. It can take up to two weeks to heal, and although in most cases the skin recovers without scarring, deeper burns can leave age spots or even scars.
Third-degree burns are deep lesions that involve all layers of the skin, including the dermis and subcutaneous tissue. The affected area becomes white, grey or charred. The skin feels dry, rough or even hard to the touch. Due to the destruction of nerve endings, the victim may not feel pain in the burn area, although pain may persist in neighbouring less damaged areas.
Blisters usually do not form in such burns, as the upper layers of the skin are destroyed. Recovery takes a long time, and in most cases, surgical intervention, including skin grafting, is required. After healing, deep scars, deformities and changes in tissue structure remain.
The most severe are fourth-degree burns, which affect not only the skin but also subcutaneous tissue, muscles, tendons and sometimes bones. Such injuries often occur during fires, accidents, contact with molten metal or high-voltage electric shocks. The affected area looks like charred or blackened tissue, sometimes with signs of carbonisation.
Due to the destruction of nerve endings, sensitivity is completely absent. This is an extremely dangerous type of burn that often requires immediate surgery, intensive care and even amputation of the affected limbs.
Understanding the symptoms of each degree of burn allows you to quickly assess the situation and determine whether you can help yourself or whether emergency medical care is required. It is important to remember that even if there is little or no pain, deep burns can be deadly due to the risk of infection, fluid loss, shock or damage to internal organs.
In the following sections, we will look in detail at how to provide first aid for burns of varying degrees to minimise the risks to the health and life of the victims.
What to do with burns at different stages?
Providing the right first aid for burns is a critical step that can have a significant impact on the victim's further condition, healing rate and risk of complications.
Burns of varying degrees require different treatment approaches, as actions that are effective for light injuries can be not only ineffective but also dangerous in severe injuries.
In this section, we will look at the algorithm of actions for each stage of burns so that you can quickly and effectively help yourself or another person in a critical situation. Knowing the right steps will help reduce pain, prevent complications and even save lives.
Burn of the 1st degree
A first-degree burn is the mildest form of burn injury that affects only the top layer of the skin - the epidermis. Such burns are usually not life-threatening and can be treated well at home. Most often, they occur as a result of short-term contact with hot objects, hot liquids, steam, or prolonged exposure to sunlight.
First aid for first-degree burns consists primarily of rapid cooling of the affected area. This can be done by rinsing the burn with cool running water at room temperature for 10-15 minutes.
The use of ice water or ice is unacceptable, as it can cause additional tissue damage due to the sharp narrowing of blood vessels. If it is not possible to cool the skin under running water, a clean, damp cloth dipped in cool water can be applied to reduce pain and discomfort.
After cooling, the skin should be gently washed with mild soap and clean water to avoid contamination and reduce the risk of infection. It is not recommended to use aggressive antiseptics, alcohol-containing solutions or hydrogen peroxide, which can irritate the skin and worsen the condition.
Next, you can apply a thin layer of petroleum jelly or aloe vera moisturiser to help retain moisture in the skin and ease the burning sensation. The use of greasy oils, butter or cosmetic creams with fragrances is not recommended as they can trap heat and interfere with the natural cooling process.
If the burn is on an area of skin that is in contact with clothing or may be subject to additional irritation, you can cover it with a clean, dry gauze bandage. It is important to avoid excessive pressure so as not to interfere with natural air circulation.
The affected area should be protected from direct sunlight to prevent re-damage. In case of severe pain, you can take an over-the-counter pain reliever, such as ibuprofen or paracetamol, following the dosage instructions.
Despite the fact that first-degree burns usually heal without complications within a few days, there are situations when you should consult a doctor. This is necessary if a large area of the body is affected, especially in children and the elderly, or if the burn is on the face, hands, feet, groin or joints.
You should also consult a medical specialist if the pain persists even after cooling down and taking painkillers, or if there are signs of infection, such as an increase in body temperature, increased redness, purulent discharge, or an unpleasant odour from the wound.
With proper care, first-degree burns usually heal without any residual marks. The skin may peel off during recovery, which is a normal process, and eventually heals without scarring or scarring. However, even with minor burns, it is important to be attentive to your condition and changes in your well-being in order to notice possible complications in time.
Burn of the 2nd degree
A second-degree burn is a serious injury that requires timely and proper first aid to reduce the risk of complications and speed up the healing process. First of all, it is important to stop the damaging factor: remove the source of heat, chemical or other factor that caused the burn. After that, you need to act quickly and carefully.
The first step in treatment is to cool the affected area. To do this, place the burned surface under cool running water at room temperature for 10-15 minutes. If running water is not available, a clean, damp compress can be used.
This will help reduce the temperature of the affected tissue, reduce pain and stop the spread of the injury. However, it is strictly forbidden to use ice water or ice, as this can cause additional damage due to vasospasm and even cause cold injury.
After cooling down, carefully remove clothing and jewellery from the affected area to avoid compression of the tissue in case of swelling. If the clothing is stuck to the skin, do not try to tear it off to avoid further damage to the tissue. In this case, cut off the loose edges of the fabric, leaving the adhering part in place.
Next, protect the burn surface from contamination. You can cover the burn with a sterile gauze cloth or a clean, dry cloth. It is important that the bandage is not too tight, as this can disrupt blood circulation and increase pain.
If blisters form on the skin, they should not be punctured or attempted to be removed, as this increases the risk of infection. Blisters perform a natural protective function by maintaining a sterile environment for tissue regeneration. If a blister bursts spontaneously, the wound should be treated with an alcohol-free antiseptic solution and covered with a sterile dressing.
To reduce pain, you can take an over-the-counter pain reliever, such as ibuprofen or paracetamol, following the recommended dosage. This will help relieve discomfort and reduce inflammation. The use of pain relieving gels or ointments without a doctor's prescription is not recommended, especially if the skin is severely damaged.
In case of a large burn area or if the affected area is located on the face, neck, hands, feet, groin or large joints, seek medical attention immediately. This also applies to burns in children, the elderly and people with chronic illnesses, as their bodies are particularly vulnerable to such injuries.
You should immediately call a doctor or go to a medical facility if the burn is accompanied by signs of general deterioration: severe pain that does not decrease after cooling and taking painkillers, fever, signs of infection (redness, pus, swelling, unpleasant odour from the wound), severe swelling or symptoms of shock (pale skin, cold sweat, weakness, impaired consciousness).
Do not apply oily substances such as oil, butter, cosmetic creams or ointments to the affected area unless medically indicated. Such products can trap heat in the tissues, creating a favourable environment for bacteria to grow, which increases the risk of infection.
Second-degree burns can take from 1 to 3 weeks to heal, depending on the depth of the lesion and proper care. In mild cases, only minor discolouration may remain after healing.
However, deeper burns can lead to scarring, especially if there was an infection or trauma to the blisters. To reduce the risk of complications, it is important to regularly examine the burned surface, keep it clean and seek medical attention to monitor the healing process if necessary.
Proper first aid has a significant impact on the prognosis of recovery from second-degree burns. Even if the injury seems minor, you should carefully monitor the condition of the wound and the general well-being of the victim, as infectious complications can develop not immediately, but several days after the injury.
Burn of the 3rd degree
A third-degree burn is a severe injury that affects all layers of the skin, including the epidermis, dermis and subcutaneous tissue, and in some cases even muscles, tendons and nerve endings. This is a serious injury that requires immediate medical attention as it can lead to serious complications, including infections, shock and even life-threatening injuries.
In the case of third-degree burns, the first priority is to ensure the safety of the victim and the caregiver. The thermal or chemical agent should be stopped, for example by extinguishing the flame or removing the heat source. If clothing is on fire, use a blanket or other dense material to extinguish the fire, avoiding the use of flammable substances.
After removing the source of the burn, it is important to assess the victim's condition. If he or she is not breathing or has no pulse, cardiopulmonary resuscitation should be started immediately. If breathing and consciousness are present, constant supervision should be provided until the arrival of medical personnel.
Call an ambulance immediately, as third-degree burns require professional treatment, including intensive care, pain relief and possible surgical intervention such as skin grafting. Do not attempt to treat such burns yourself.
It is strictly forbidden to immerse the burn in water or cool it for a long time, especially if the area is large. This can lead to hypothermia and shock. If necessary, you can gently blow cool air over the affected area to relieve pain for a short time, avoiding direct contact with water or ice.
When providing care, it is important to carefully remove loose clothing and jewellery if it is not stuck to the skin. If tissue is stuck to the affected area, it should not be torn off as this may cause further damage. Instead, cut the clothing around the burn area.
The burned area should then be covered with a sterile, dry gauze cloth or clean cloth to prevent infection. The bandage should not put pressure on the affected area, especially if there are signs of swelling. If the burn is on a limb, it is advisable to elevate it above the level of the heart to reduce swelling.
Do not apply any ointments, creams, oils or other substances to the burned area. Such actions can only worsen the situation by trapping heat and creating conditions for infection. It is also forbidden to use any home-made remedies or folk methods of treatment.
If the victim shows signs of shock - pallor, cold sweat, rapid breathing, weak pulse, dizziness or loss of consciousness - it is necessary to lay the person on their back, raise their legs about 30 cm and provide access to fresh air. Monitor the victim's breathing and cardiac activity until an ambulance arrives.
Third-degree burns are often accompanied by serious complications, such as loss of large amounts of fluid, which can lead to dehydration and shock. Therefore, it is important not to allow the victim to eat or drink, especially if there is a suspicion of airway damage or the need for surgery.
Treatment of such burns is always carried out in a hospital. It includes infusion therapy to restore fluid volume, pain relief, infection prevention, and surgical treatment of wounds. In many cases, skin grafting is required to restore damaged tissue.
A third-degree burn is an extremely serious injury that threatens the victim's life. Proper first aid can significantly reduce the risk of complications and increase the chances of a successful recovery. The key is to act calmly, quickly and efficiently, keeping in mind the safety of both the victim and the person providing assistance.
Remedies for burns
The treatment of burns depends on the extent of the skin damage and the conditions in which care is provided. At home or in the field, it is important not only to provide first aid, but also to choose effective products that will help reduce pain, prevent infection and speed up the healing process. Depending on the severity of the injury, different products are used: creams, gels, sprays and special anti-burn dressings.
For minor injuries, such as first-degree burns or mild thermal injuries (e.g. short-term contact with a hot object), dexpanthenol creams are well suited. This substance promotes skin regeneration, relieves inflammation and reduces irritation. Such products help to moisturise the damaged area and create a protective barrier that prevents moisture loss.
Creams such as Levomecol or "Rescuer" are also effective for light burns. Levomecol has pronounced antibacterial properties and helps prevent the development of infections in superficial wounds. It is often used to treat minor injuries, especially if there is a risk of wound contamination.
Thanks to its regenerative properties, "Rescuer" can reduce inflammation and promote faster skin healing. However, in case of more serious burns (second and higher degrees), these creams can only be used as an aid - they should not be considered as the main treatment.
In the case of second-degree burns, when blisters and severe swelling appear on the skin, sprays or gels with a cooling effect, such as hydrogel dressings, can be more effective. They are well absorbed into the skin, have anti-inflammatory and analgesic effects, which helps to reduce pain and prevent infection.
One of these products is the Burnshield 100x100 mm anti-burn dressing, which provides effective cooling of the damaged area, relieves pain and prevents the burn from deepening. Thanks to its structure, it maintains a moist environment conducive to healing and reduces the risk of scarring.
Another effective solution for the field is the Burncare 100x100 mm burn dressing. It is ideal for protecting wounds outdoors by creating a barrier against dirt and dust. The bandage contains a special gel that not only moisturises the skin but also has an antimicrobial effect, which is especially important in cases where it is not possible to provide sterile conditions.
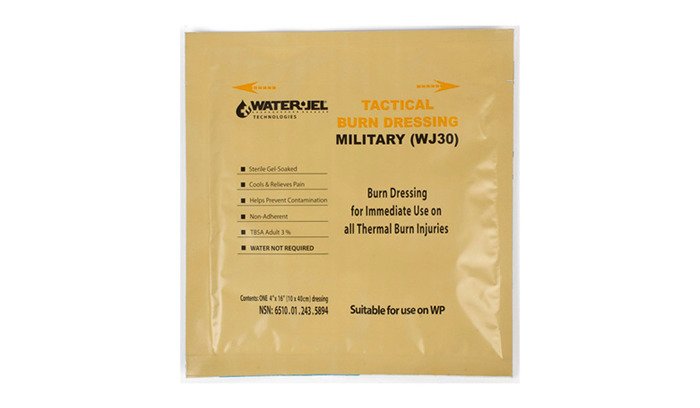
For more extensive burn injuries, the Water-Jel WJ30HA 100x400 mm burn dressing will be effective. Due to its large size, it is suitable for treating burns on the arms, legs and back, providing not only cooling but also reliable protection against external irritants. This bandage is indispensable in the field, where it is important to respond quickly to a burn injury and ensure the victim's stable condition until medical assistance arrives.
In cases where an even larger area needs to be covered, such as chest, back or thigh burns, the Burnshield 200x200 mm burn dressing is recommended. It ensures that the cooling gel is evenly distributed over the entire surface of the injury, helping to reduce pain, swelling and prevent the spread of infection. It can be used in medical facilities, in the field or at home.
For third- and fourth-degree burns, the use of topical agents should be minimal and only as part of comprehensive medical care. In such cases, it is important to take the victim to a medical facility immediately for appropriate treatment, including infusion therapy, pain relief and surgery.
Regardless of the extent of the burn, there are some important rules to keep in mind. Do not apply oily substances such as oil, butter or cosmetic creams to burns, as they trap heat and can aggravate tissue damage. It is also not recommended to use alcohol solutions, which can further irritate the skin.
The right choice of burn treatment depends on the specific situation, the severity of the injury and the conditions present. In mild cases, moisturising creams or gels may be sufficient, while in severe situations, comprehensive medical care with the use of specialised burn materials is required. It is always important to closely monitor the condition of the wound and the general well-being of the victim in order to notice signs of complications and seek medical attention in time.
If you are looking for reliable first aid products for burns, we recommend that you pay attention to the range of our tactical medicine store, where you will find certified products for effective assistance in extreme conditions.
What not to use for burn treatment
When providing first aid for burns, it is important not only to know what to do, but also to clearly understand what actions and products to avoid. Incorrect treatment can not only fail to help, but also worsen the situation, increase pain, increase the depth of the injury or even cause infectious complications. Below is a list of products that are strictly not recommended for the treatment of burns:
- Ice or ice packs. Direct contact of ice with burned skin can cause additional tissue damage. Ice causes a sharp constriction of blood vessels, which impairs blood circulation and slows down the healing process. In addition, there is a risk of developing a cold burn, which will further complicate treatment. Instead of ice, use cool water to gently cool the affected area.
- Oil, oil products and fat creams. The use of vegetable oil, butter or fatty creams creates a dense barrier on the skin that traps heat and increases the depth of the burn injury. In addition, oil products can promote the growth of bacteria, which increases the risk of wound infection.
- Urine. Although urine was sometimes recommended for wound care in the past, modern medicine strongly discourages this practice. Urine can contain microorganisms that enter open wounds, causing infectious complications. Its use has no proven benefit in the treatment of burns.
- Powders, special powders or antibiotic ointments without consulting a doctor. Unauthorised use of antibacterial ointments or powders can cause allergic reactions, skin irritation or even contribute to the development of antibiotic resistance. Treatment with antibacterial agents should be carried out only on the recommendation of a medical professional, especially in the case of deep or infected burns.
- Chlorhexidine, iodine and other aggressive antiseptics. Applying chlorhexidine, iodine or brilliant green directly to the burn surface can cause additional skin irritation, dry out the tissue and slow down the healing process. These antiseptics can be useful for treating the skin around the burn, but not the wound itself. They should be used only after consulting a doctor.
- Honey, toothpaste and other "folk remedies". Using honey or toothpaste to treat burns is another dangerous myth. Such substances can cause irritation, allergic reactions and create a favourable environment for bacterial growth. It is especially dangerous to apply them to open wounds or areas with damaged skin.
- Vinegar, alcohol or other chemicals. Contact of burnt skin with harsh chemicals such as vinegar or alcohol can increase irritation, cause chemical burns and significantly deteriorate tissue. Instead, use sterile saline or clean water to flush the wound.
Improper treatment of burns can lead to serious consequences, such as infection, deep scarring, delayed healing or even systemic complications. The use of the products on this list is often based on folk myths that have no medical basis.
If you are in doubt about the correct approach to treating a burn, it is better to seek medical help or consult a specialist. Even mild burns can become more severe if they are not treated properly, so it is important to act carefully and responsibly.
Remember: the best first aid for burns is to cool the affected area with cool water, protect it from further damage and seek medical attention in a timely manner if necessary.
Conclusion: preventive tips
Burns are one of the most common injuries both at home and in extreme conditions. However, in most cases, they can be avoided by following simple safety precautions. Prevention of burns is based on attentiveness, creating a safe environment and following basic rules for handling heat sources, chemicals and electrical appliances.
In the home, one of the key risks is carelessness in the kitchen. Never leave cooking unattended, even if you think you have everything under control. Pans should be positioned with their handles facing the inside of the stove to reduce the risk of accidentally knocking over hot food. It is better to place hot drinks and liquids out of the reach of children, as boiling water is one of the main causes of thermal burns in children.
It is equally important to avoid storing electrical appliances near water sources to prevent not only burns but also electrical injuries. Be especially careful when handling household appliances: always switch them off after use, check for proper functioning and do not leave them on unnecessarily.
To protect children from household dangers, you should restrict their access to electrical and gas appliances. Make sure that protective caps are always fitted to sockets that are not in use. Sources of open flame, such as matches and lighters, should be kept out of the reach of children.
You should also install smoke detectors in your home and regularly check their functioning, replacing the batteries if necessary. Having a fire extinguisher at home is another important element of basic safety, as it can save lives in an emergency.
Special attention should be paid to preventing chemical burns. Chemicals should be stored in securely closed containers out of the reach of children and pets. When using aggressive chemicals for cleaning or repair, be sure to follow the instructions on the packaging and wear protective gloves and goggles.
When it comes to preventing sunburn, it is important to remember to protect your skin in the summer. Use sunscreens with a high SPF, especially if you plan to spend long periods of time in the sun. Wear protective clothing, hats and avoid exposure to the sun during the hours of highest UV activity - from 11:00 to 16:00.
Also remember the basic safety rules for handling hot objects. Wear heat-protective gloves, especially when cooking or working with hot surfaces. Hot drinks should not be left on the edge of a table or on unstable surfaces where they can easily be knocked over.
In general, burn prevention is based on simple but important rules: be careful, control potentially dangerous situations and provide a safe environment for yourself and your loved ones. Following these recommendations will help to significantly reduce the risk of burn injuries and make your life safer.